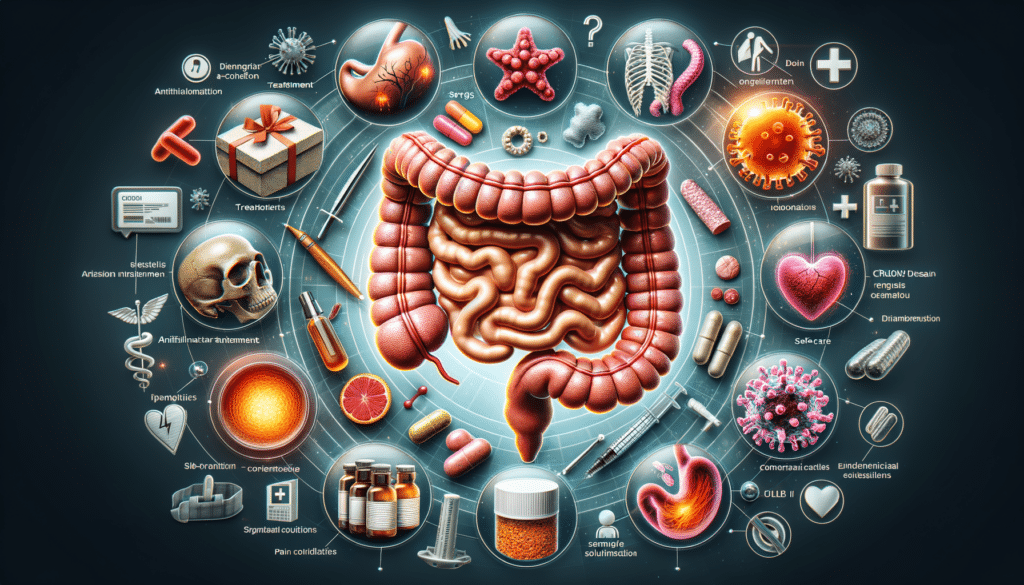
Managing Crohn’s Disease: An Overview
Managing Crohn’s disease requires a multifaceted approach that combines medical treatments, lifestyle changes, and self-care strategies. This chronic inflammatory bowel disease (IBD) can vary significantly in severity and symptoms from one person to another, making personalized management plans essential. The primary goal in managing Crohn’s is to reduce inflammation, alleviate symptoms, and maintain remission.
Key components of managing Crohn’s disease include:
- Medication: Anti-inflammatory drugs, immunosuppressants, and biologics are commonly prescribed to control inflammation and immune response.
- Dietary Adjustments: Identifying and avoiding trigger foods can help minimize flare-ups. A balanced, nutrient-rich diet supports overall health.
- Stress Management: Stress can exacerbate symptoms, so incorporating stress-reducing techniques like yoga, meditation, or therapy is beneficial.
- Regular Monitoring: Regular check-ups with healthcare professionals are crucial to monitor disease progression and adjust treatments as needed.
Incorporating these elements into daily life can help individuals manage their symptoms more effectively, improving their quality of life. It’s important to work closely with healthcare providers to develop a comprehensive management plan tailored to individual needs.
Crohn’s Disease Symptoms and Signs
Crohn’s disease symptoms can be unpredictable and vary widely among individuals. Recognizing these symptoms early can lead to timely intervention and better management. Common symptoms include:
- Abdominal Pain: Often crampy and can range from mild to severe.
- Diarrhea: Frequent, urgent bowel movements that may contain blood or mucus.
- Fatigue: Persistent tiredness that doesn’t improve with rest.
- Weight Loss: Unintentional weight loss due to malabsorption or reduced appetite.
- Fever: Low-grade fever may accompany flare-ups.
In addition to gastrointestinal symptoms, Crohn’s disease can cause extraintestinal manifestations such as joint pain, skin rashes, and eye inflammation. These signs highlight the systemic nature of the disease, necessitating a holistic approach to treatment.
Understanding these symptoms helps in distinguishing Crohn’s from other gastrointestinal disorders, allowing for more accurate diagnosis and treatment. Keeping a symptom diary can be helpful for patients to track their symptoms and identify potential triggers.
Treatment for Mild Crohn’s Disease
Treating mild Crohn’s disease involves a combination of lifestyle changes and medication aimed at controlling inflammation and maintaining remission. For those with milder forms of the disease, the treatment approach may include:
- 5-ASA Compounds: These anti-inflammatory drugs are often used as first-line treatment for mild cases.
- Dietary Modifications: A low-fiber or low-residue diet can help reduce symptoms by minimizing bowel irritation.
- Probiotics: These can support gut health by balancing intestinal flora.
- Regular Exercise: Physical activity can improve overall health and reduce stress, which may alleviate symptoms.
For individuals with mild Crohn’s, close monitoring is essential to detect any changes in disease activity. Regular consultations with healthcare providers ensure that treatment plans are adjusted appropriately, preventing escalation of symptoms.
While mild Crohn’s may not require aggressive treatment, it is important to remain vigilant and proactive in managing the condition to prevent progression and maintain quality of life.