Recognizing the Signs and Symptoms of Crohn’s Disease
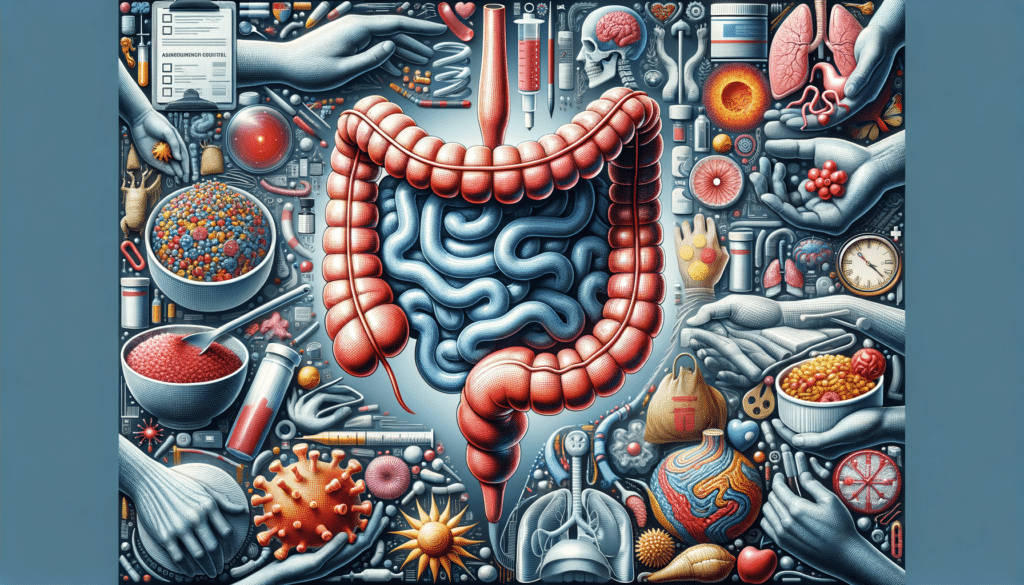
Crohn’s disease, a type of inflammatory bowel disease (IBD), manifests in various ways, making it a challenging condition to diagnose. Common symptoms include persistent diarrhea, abdominal pain, and cramping, often leading to unintended weight loss and fatigue. These symptoms can vary in intensity and may come and go, leading to periods of flare-ups and remission. It’s crucial to recognize these signs early, as they can significantly impact daily life.
Beyond the digestive symptoms, Crohn’s disease can also cause inflammation in other parts of the body. Some individuals experience joint pain, skin rashes, and even eye inflammation. This systemic nature of the disease underscores the importance of a comprehensive approach to diagnosis and management.
While these symptoms might suggest Crohn’s disease, they overlap with other gastrointestinal conditions, necessitating thorough medical evaluation. Diagnostic tools like colonoscopy, MRI, and blood tests help in confirming the presence of Crohn’s. Early detection is key, as it allows for timely intervention, potentially reducing the severity of future flare-ups.
Exploring Treatment Options for Crohn’s Disease
Treatment for Crohn’s disease is multifaceted, aiming to reduce inflammation, manage symptoms, and maintain remission. Medications form the cornerstone of treatment, with options ranging from anti-inflammatory drugs to immune system suppressors. These medications help in controlling the inflammatory response that characterizes Crohn’s disease.
For those with mild Crohn’s disease, lifestyle modifications and dietary adjustments often play a significant role. A diet rich in nutrients and tailored to avoid trigger foods can alleviate symptoms and support overall health. In some cases, nutritional supplements may be recommended to address deficiencies caused by malabsorption.
In more severe cases, where medications and lifestyle changes are insufficient, surgical interventions may be necessary. Surgery can remove damaged sections of the digestive tract, providing relief and improving quality of life. However, this is typically considered a last resort after other treatments have been exhausted.
It’s essential for individuals with Crohn’s disease to work closely with their healthcare providers to develop a personalized treatment plan. This collaborative approach ensures that treatment strategies are tailored to the individual’s specific needs and disease severity.
Effective Self-Care Strategies for Managing Crohn’s Disease
Self-care is a vital component of managing Crohn’s disease, complementing medical treatments and helping individuals maintain a higher quality of life. One of the fundamental aspects of self-care is dietary management. Keeping a food diary can help identify foods that trigger symptoms, allowing for adjustments that minimize flare-ups.
Stress management is another critical area, as stress can exacerbate symptoms. Techniques such as mindfulness, meditation, and yoga have been shown to reduce stress levels and improve overall well-being. Regular physical activity, tailored to the individual’s capabilities, can also promote digestive health and reduce stress.
Staying informed about the condition and actively participating in healthcare decisions empowers individuals to better manage their disease. Support groups and counseling can provide emotional support and practical advice from others who understand the challenges of living with Crohn’s disease.
Ultimately, self-care involves a proactive approach, integrating healthy habits into daily routines and seeking support when needed. By taking an active role in managing their health, individuals with Crohn’s disease can improve their quality of life and reduce the impact of the disease on their daily activities.