Understanding Crohn’s Disease: Symptoms and Signs
Crohn’s disease is a chronic inflammatory condition of the gastrointestinal tract, part of a group of diseases known as inflammatory bowel disease (IBD). Symptoms can vary widely among individuals, but common signs include persistent diarrhea, abdominal pain, and weight loss. Some individuals may experience fatigue, fever, and reduced appetite. The inflammation caused by Crohn’s disease can affect different areas of the digestive tract in different people, leading to a range of symptoms.
Recognizing the signs early is crucial for managing the disease effectively. Key indicators often include:
- Abdominal Pain: Often localized in the lower right quadrant, resembling appendicitis.
- Diarrhea: Frequent and urgent bowel movements can lead to dehydration.
- Weight Loss: Due to malabsorption of nutrients.
- Fatigue: Chronic inflammation can lead to feelings of exhaustion.
Understanding these symptoms helps in seeking timely medical advice, which is essential for preventing complications. While these signs are common, they can also be indicative of other conditions, making professional evaluation important.
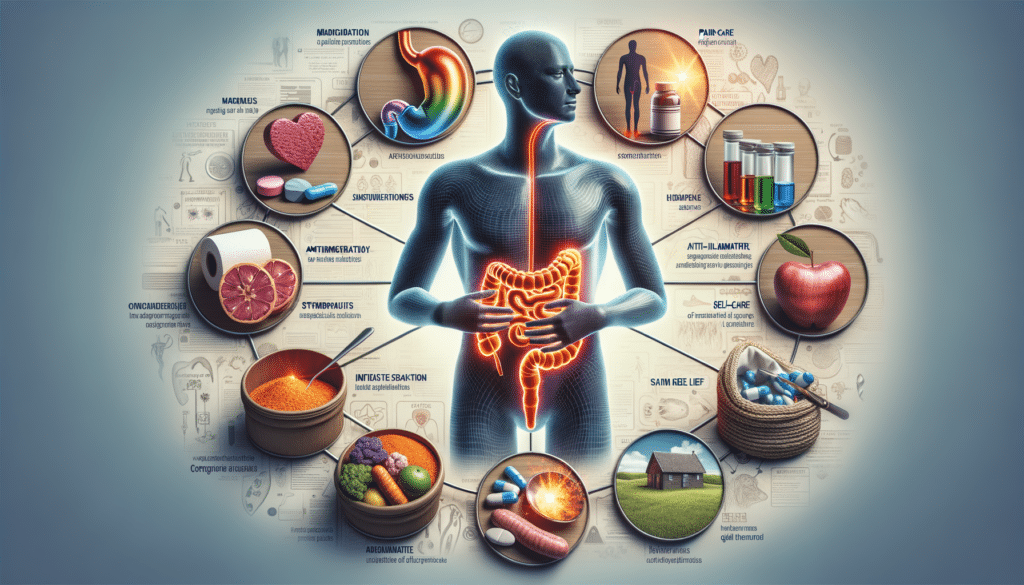
Treatment Options for Crohn’s Disease
Treating Crohn’s disease involves a multifaceted approach aimed at reducing inflammation, managing symptoms, and achieving long-term remission. Treatment plans are often personalized, depending on the severity and location of the disease. Here are some common treatment strategies:
- Medications: Anti-inflammatory drugs, such as aminosalicylates and corticosteroids, are often used to reduce inflammation. Immunosuppressants may also be prescribed to decrease the immune system’s activity.
- Biologic Therapies: These are targeted therapies that block specific proteins in the body that cause inflammation.
- Nutritional Support: Special diets or nutritional supplements can help manage symptoms and ensure adequate nutrient intake.
- Surgery: In cases where medication and lifestyle changes do not control symptoms, surgery may be necessary to remove damaged portions of the digestive tract.
Each treatment option has its benefits and potential side effects. Consulting with a healthcare provider is essential to tailor the treatment plan to the individual’s specific needs and lifestyle.
Self-Care and Pain Relief for Crohn’s Disease
Self-care is a vital component of managing Crohn’s disease, helping to alleviate symptoms and improve quality of life. Here are some strategies:
- Dietary Adjustments: Identifying and avoiding trigger foods can reduce symptoms. A diet low in fiber may be recommended during flare-ups to ease digestion.
- Stress Management: Stress can exacerbate symptoms, so techniques such as meditation, yoga, or counseling can be beneficial.
- Regular Exercise: Engaging in low-impact activities like walking or swimming can help maintain overall health and reduce stress.
- Pain Relief: Over-the-counter pain relievers may help, but it’s important to consult a doctor to avoid medications that can worsen symptoms.
Incorporating these self-care practices can significantly impact one’s ability to manage Crohn’s disease effectively. It’s about finding a balance that works for the individual, often requiring some trial and error.