Recognizing Sézary Syndrome and Exploring Treatment Options
Understanding Sézary Syndrome: Symptoms and Skin Condition
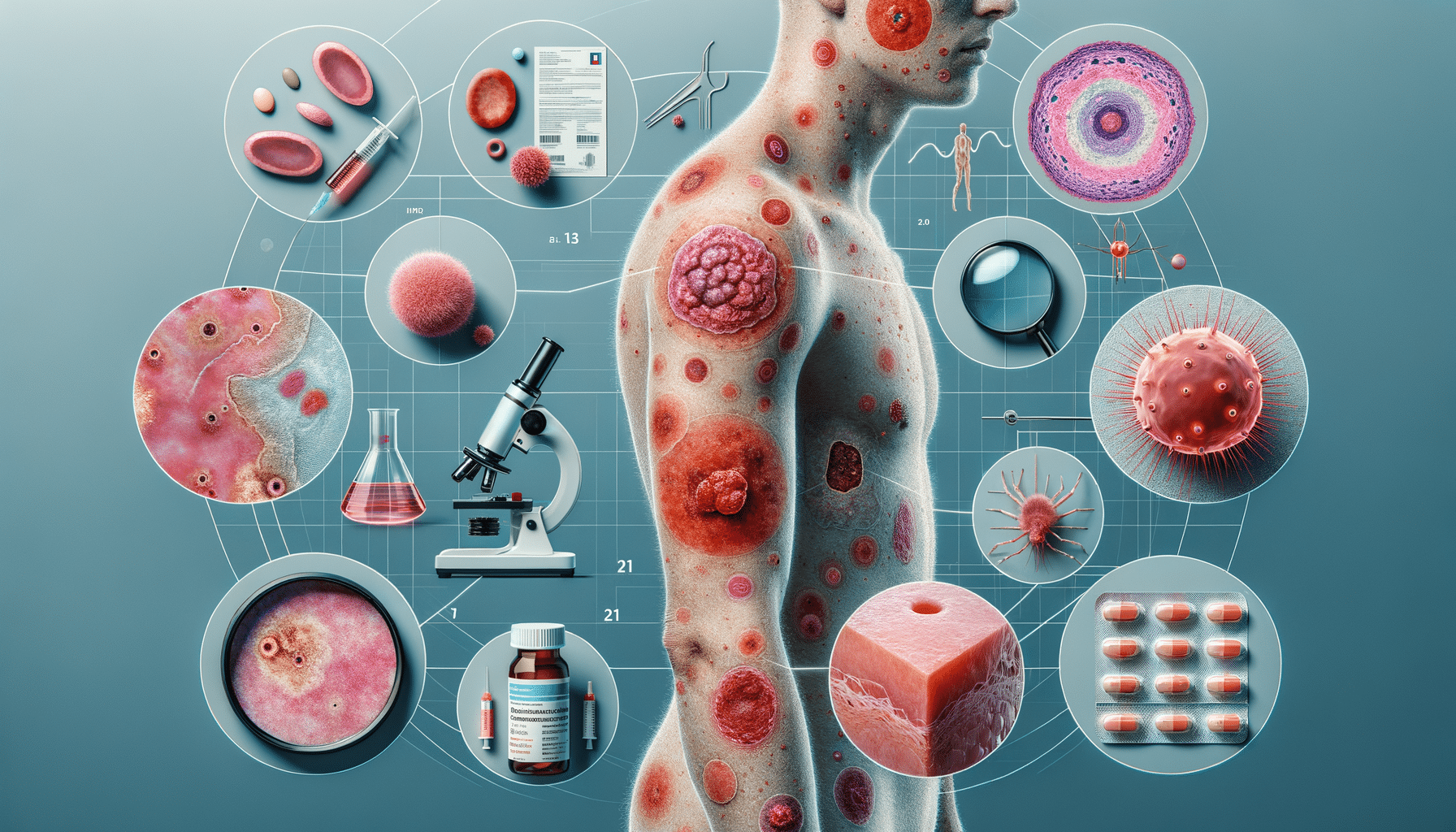
Sézary Syndrome is a rare and aggressive form of cutaneous T-cell lymphoma that primarily affects the skin, blood, and lymph nodes. This condition is characterized by the triad of erythroderma, lymphadenopathy, and atypical circulating lymphocytes known as Sézary cells. The skin manifestations are often the most noticeable symptoms and can include widespread redness, scaling, and itching, which may be mistaken for other dermatological conditions such as eczema or psoriasis.
Patients with Sézary Syndrome often experience additional symptoms such as thickened skin on the palms and soles, hair loss, and nail abnormalities. The persistent and severe itching can significantly affect the quality of life, leading to sleep disturbances and emotional distress. Understanding these symptoms is crucial for early detection and diagnosis, as the condition can be easily misdiagnosed due to its resemblance to other skin disorders.
Unlike other skin conditions, Sézary Syndrome involves systemic symptoms due to the infiltration of malignant T-cells in the blood. Patients may experience fevers, night sweats, and significant weight loss. The presence of these systemic symptoms, along with the characteristic skin changes, should prompt further investigation and referral to a specialist for a definitive diagnosis.
Diagnosing and Managing Sézary Syndrome
The diagnosis of Sézary Syndrome is complex and requires a combination of clinical evaluation, laboratory tests, and biopsies. A dermatologist or oncologist may perform a skin biopsy to examine the presence of atypical lymphocytes in the skin. Blood tests are also crucial to detect Sézary cells in the bloodstream and assess the extent of the disease. Flow cytometry and immunophenotyping are often used to differentiate Sézary Syndrome from other types of cutaneous T-cell lymphomas.
Management of Sézary Syndrome involves a multidisciplinary approach, often requiring the expertise of dermatologists, oncologists, and hematologists. Treatment options can vary depending on the stage and severity of the disease, as well as the patient’s overall health. Common treatments include phototherapy, systemic therapies such as retinoids or histone deacetylase inhibitors, and immunotherapy. In some cases, chemotherapy or stem cell transplantation may be considered for more advanced stages.
Supportive care is also an essential component of the management strategy. Patients may benefit from emollients and topical steroids to alleviate skin symptoms, while antihistamines can help manage itching. Psychological support and counseling can be valuable for patients dealing with the emotional impact of a chronic and potentially life-threatening illness.
Exploring Rare Skin Lymphomas: Beyond Sézary Syndrome
Sézary Syndrome is part of a broader category of rare skin lymphomas known as cutaneous T-cell lymphomas (CTCLs). These lymphomas are characterized by the presence of malignant T-cells in the skin and can present with a variety of symptoms ranging from localized patches and plaques to more widespread erythroderma, as seen in Sézary Syndrome.
Other types of CTCLs include mycosis fungoides, which is the most common form and typically presents with patches, plaques, and tumors on the skin. In contrast, Sézary Syndrome is more aggressive and systemic, often requiring more intensive treatment. Despite their differences, these conditions share some overlapping features, which can pose diagnostic challenges.
Research into rare skin lymphomas is ongoing, with efforts to better understand their pathogenesis and develop targeted therapies. Advances in molecular biology and genomics are paving the way for personalized medicine approaches, offering hope for more effective and tailored treatments for patients with these rare and challenging conditions.