A Helpful Overview of Ulcerative Colitis Treatment Options in 2025
Understanding Ulcerative Colitis Treatment Options
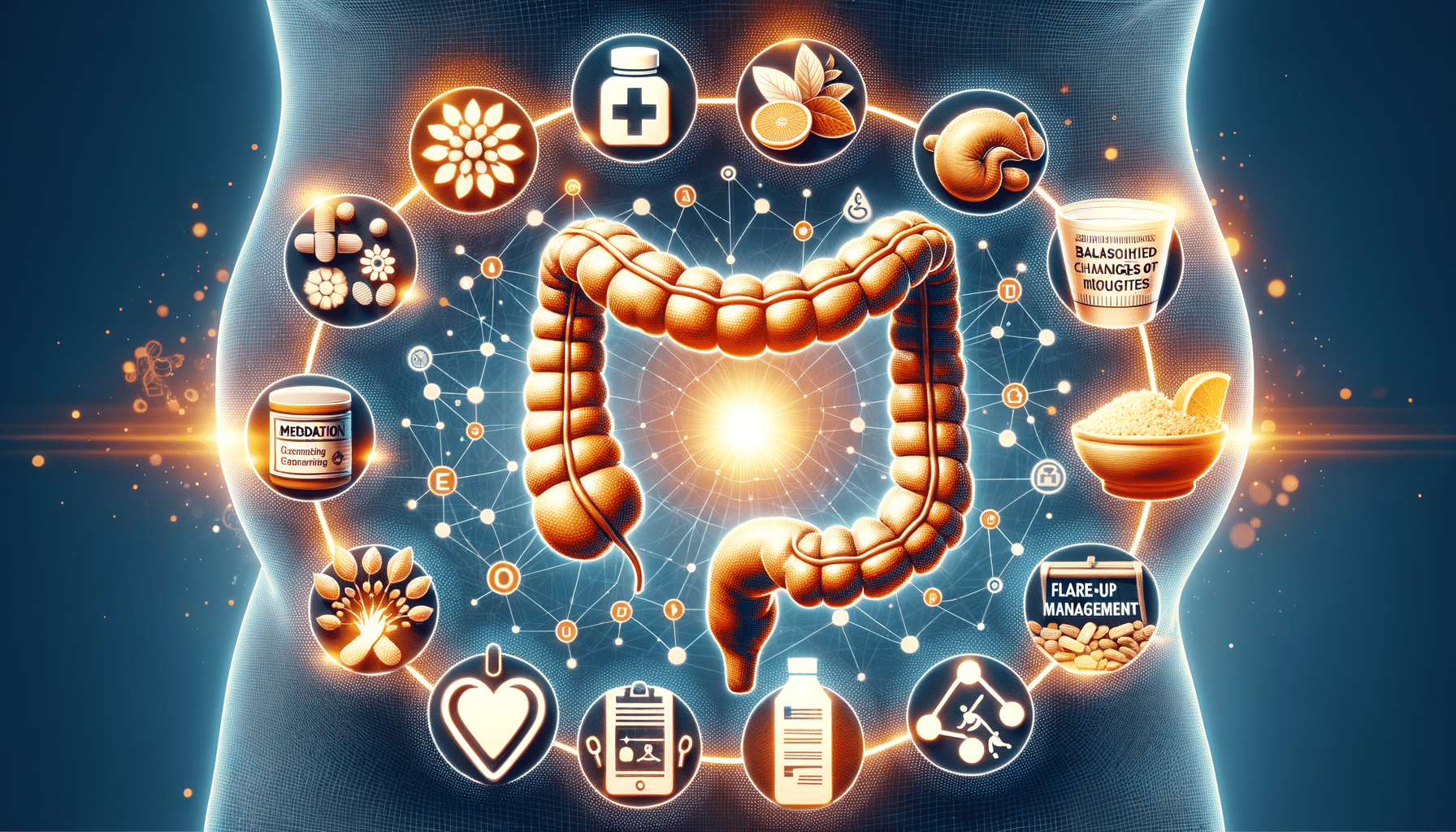
Ulcerative colitis (UC) is a chronic inflammatory bowel disease that can significantly impact a person’s quality of life. Understanding the treatment options available is crucial for managing the condition effectively. Treatments for UC are generally aimed at reducing inflammation, controlling symptoms, and preventing flare-ups. The treatment plan is often personalized, taking into account the severity of the condition, the patient’s overall health, and their response to previous treatments.
There are several categories of treatments available for UC, including:
- Medications: These are typically the first line of treatment and include aminosalicylates, corticosteroids, immunomodulators, and biologics. Each medication works differently, and the choice often depends on the severity of the disease and the patient’s response to previous treatments.
- Surgery: In cases where medication is not effective, surgery may be considered. This often involves removing the colon and rectum, a procedure known as a proctocolectomy.
- Lifestyle Changes: Adjustments in diet, stress management, and exercise can play a supportive role in managing symptoms and improving overall health.
Understanding these options and working closely with healthcare providers can empower patients to make informed decisions about their care. Regular monitoring and adjustments to the treatment plan may be necessary to achieve the best outcomes.
Treatments for Managing UC Flare-Ups
Managing flare-ups is a critical aspect of living with ulcerative colitis. Flare-ups can be unpredictable and vary in intensity, making it essential for patients to have a plan in place. Immediate treatment often involves medications to quickly reduce inflammation and control symptoms.
During a flare-up, doctors may prescribe:
- Corticosteroids: These are fast-acting anti-inflammatory drugs that help reduce symptoms quickly. However, they are typically used for short-term management due to potential side effects.
- Biologics: These are newer medications that target specific components of the immune system. They can be effective in controlling moderate to severe flare-ups.
In addition to medication, patients may need to adjust their diet temporarily to avoid foods that can exacerbate symptoms. Staying hydrated and getting adequate rest are also important during this time.
Communication with healthcare providers is crucial during a flare-up. Patients should report any changes in symptoms or side effects from medications. Together with their healthcare team, patients can adjust their treatment plan to manage flare-ups effectively and minimize their impact on daily life.
Lifestyle Changes That May Help UC Symptoms
While medications are central to managing ulcerative colitis, lifestyle changes can also play a significant role in alleviating symptoms and improving overall well-being. These changes can complement medical treatments and help maintain remission.
Some lifestyle adjustments that may benefit UC patients include:
- Dietary Modifications: Identifying and avoiding trigger foods is crucial. Some patients find relief by following a low-residue diet during flare-ups, which limits high-fiber foods that can irritate the bowel.
- Stress Management: Stress can exacerbate UC symptoms, so incorporating stress-reducing practices like yoga, meditation, or deep-breathing exercises can be beneficial.
- Regular Exercise: Engaging in regular physical activity can improve overall health, reduce stress, and enhance mood, which may help manage UC symptoms.
Patients are encouraged to work with healthcare providers to develop personalized lifestyle plans. These plans should consider individual triggers, preferences, and health goals. By integrating these changes, patients can potentially reduce the frequency and severity of flare-ups and improve their quality of life.