Here’s Why More People Are Exploring Ulcerative Colitis
Early Signs of Ulcerative Colitis in 2025
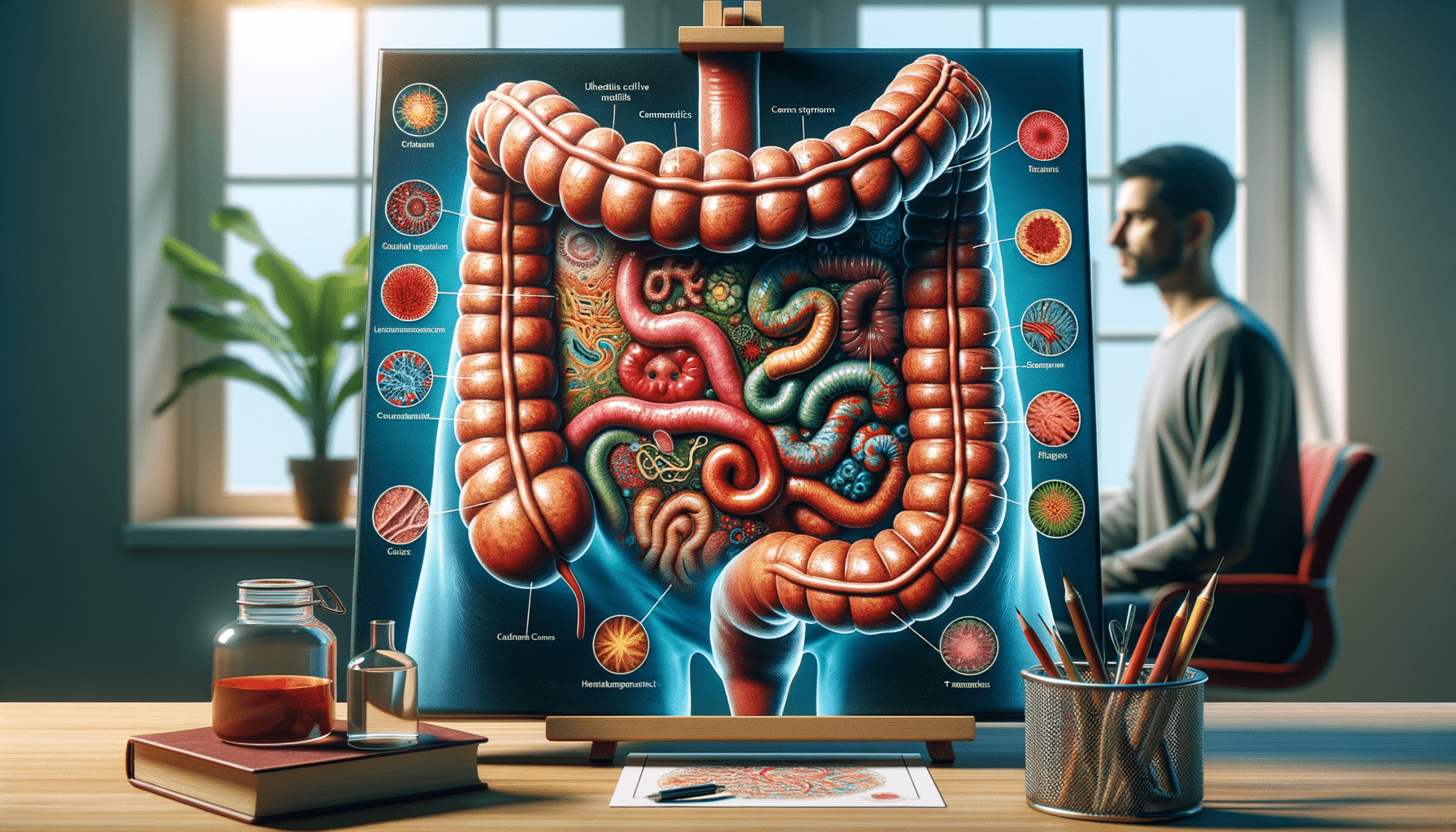
In 2025, the early signs of ulcerative colitis (UC) continue to be a subject of significant interest, especially as awareness around digestive health grows. Many individuals first notice subtle changes in their bowel habits, such as increased frequency, urgency, or the presence of blood in the stool. These symptoms can often be mistaken for other digestive issues, leading to delays in diagnosis. However, advancements in medical technology have made it easier to identify these early signs, allowing for quicker intervention.
Another early indicator of UC is abdominal pain and cramping, which may initially be mild but can escalate over time. Patients often report a feeling of incomplete evacuation after using the restroom, contributing to discomfort and anxiety. Fatigue is also a common early symptom, sometimes overlooked as it can be attributed to various other factors.
In recent years, there has been a growing recognition of the role that lifestyle and diet play in the onset of UC symptoms. Stress, dietary choices, and even environmental factors are being studied for their potential impact on the development of UC. As such, individuals are encouraged to monitor their symptoms closely and seek medical advice if they notice persistent changes in their digestive health.
Common Symptoms of Ulcerative Colitis
Ulcerative colitis manifests through a range of symptoms that can vary in severity from one individual to another. Common symptoms include persistent diarrhea, often accompanied by blood or pus, which can lead to dehydration and weight loss. Abdominal pain and cramping are also prevalent, often occurring before bowel movements.
Fatigue is another notable symptom, affecting many individuals with UC. This exhaustion can be attributed to the body’s constant battle with inflammation and the resultant nutrient deficiencies. Anemia, resulting from blood loss in the stool, further exacerbates feelings of tiredness.
Outside the digestive tract, UC can cause symptoms such as joint pain, skin rashes, and eye inflammation. These extra-intestinal manifestations highlight the systemic nature of the disease and the importance of a holistic approach to treatment. Patients often experience varying degrees of these symptoms, with periods of remission and flare-ups.
Understanding these symptoms is crucial for managing UC effectively. Patients are encouraged to keep a detailed record of their symptoms, noting any triggers or patterns, which can be invaluable during consultations with healthcare providers.
Exploring Treatment Options for Ulcerative Colitis
Treatment for ulcerative colitis has evolved significantly, offering patients a range of options tailored to their specific needs. The primary goal of treatment is to reduce inflammation, manage symptoms, and achieve long-term remission. Medications remain a cornerstone of UC treatment, with options including aminosalicylates, corticosteroids, immunomodulators, and biologics.
Aminosalicylates are often the first line of treatment for mild to moderate UC, helping to reduce inflammation in the colon. For more severe cases, corticosteroids may be prescribed to quickly control inflammation, although they are not suitable for long-term use due to potential side effects. Immunomodulators and biologics are used for patients who do not respond to conventional therapies, targeting specific components of the immune system to control inflammation.
In addition to medication, lifestyle modifications play a crucial role in managing UC. A balanced diet, stress management, and regular exercise can help alleviate symptoms and improve overall well-being. Some patients explore complementary therapies such as probiotics, acupuncture, or herbal supplements, although these should be discussed with a healthcare provider to ensure safety and efficacy.
Surgery may be considered for patients with severe UC who do not respond to medical treatments. Procedures such as colectomy or ileal pouch-anal anastomosis can offer relief and improve quality of life. The decision to undergo surgery is complex and involves careful consideration of the risks and benefits.