Early Signs of Ulcerative Colitis in 2025
In 2025, the early signs of ulcerative colitis (UC) are becoming increasingly recognized due to heightened awareness and improved diagnostic techniques. Individuals are more informed about the subtle symptoms that might indicate the onset of UC. Early signs often include persistent diarrhea, abdominal pain, and rectal bleeding. These symptoms can be mistaken for other gastrointestinal issues, but their persistence and severity often prompt further investigation.
Advancements in medical technology have made it easier to detect UC earlier. Non-invasive tests such as fecal calprotectin and advanced imaging techniques are being used more frequently, allowing for earlier intervention. Patients are encouraged to seek medical advice if they experience symptoms like unexplained weight loss, fatigue, or a sudden change in bowel habits. These indicators, when combined with family history, can provide a clearer picture of the likelihood of developing UC.
Public health campaigns are also playing a role in educating the public about UC. These initiatives aim to reduce the stigma associated with digestive disorders and encourage individuals to seek help without delay. As a result, more people are recognizing the importance of early diagnosis, which can significantly improve management and quality of life.
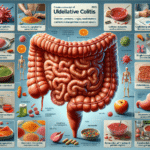
Common Symptoms of Ulcerative Colitis
Understanding the common symptoms of ulcerative colitis is crucial for early detection and effective management. UC primarily affects the colon and rectum, leading to a range of gastrointestinal symptoms. The most prevalent signs include:
- Chronic diarrhea, often with blood or pus
- Abdominal pain and cramping
- Urgency to defecate
- Fatigue and weakness
- Unintended weight loss
These symptoms can vary in intensity and frequency, often correlating with periods of flare-ups and remission. During a flare-up, symptoms can become more severe, leading to increased discomfort and disruption of daily life. Conversely, periods of remission may bring relief, with symptoms subsiding or disappearing temporarily.
Extraintestinal symptoms can also occur, affecting other parts of the body. These may include joint pain, skin rashes, and eye inflammation, which are often linked to the systemic nature of the disease. Recognizing these symptoms is essential for comprehensive management, as they can provide clues to the underlying inflammatory processes associated with UC.
In 2025, increased awareness and understanding of these symptoms are helping patients and healthcare providers to identify UC more quickly, leading to timely treatment and better outcomes.
Exploring Treatment Options for Ulcerative Colitis
In 2025, the landscape of treatment options for ulcerative colitis is more diverse and promising than ever. With ongoing research and development, patients have access to a range of therapeutic strategies aimed at managing symptoms and improving quality of life.
Conventional treatments remain a cornerstone in UC management. These include:
- Aminosalicylates, which help reduce inflammation in the colon
- Corticosteroids, used for short-term control of flare-ups
- Immunosuppressants, which modulate the immune response
- Biologics, targeting specific pathways in the inflammatory process
In addition to these, newer therapies are emerging. Small molecule drugs, which target specific proteins involved in inflammation, are gaining attention for their effectiveness and potential for fewer side effects. Moreover, advancements in personalized medicine are allowing treatments to be tailored to individual genetic profiles, improving efficacy and reducing adverse reactions.
Patients are also exploring complementary and alternative therapies. These include dietary modifications, probiotics, and mind-body interventions such as yoga and meditation. While these approaches may not replace conventional treatments, they can offer additional support and symptom relief.
As research continues, the hope is to develop even more targeted therapies that address the root causes of UC, ultimately leading to more sustained remission and improved patient outcomes.