Early Signs of Ulcerative Colitis in 2025
In 2025, the early signs of ulcerative colitis (UC) are gaining attention as more individuals become health-conscious and proactive about their digestive health. Recognizing these signs early can significantly impact the management and treatment of the condition. Common early indicators include persistent diarrhea, often accompanied by blood or pus, abdominal pain, and an urgent need to defecate. These symptoms can be mistaken for other gastrointestinal issues, making early diagnosis a challenge.
With advancements in medical technology, healthcare professionals are now better equipped to detect UC at its onset. Genetic testing and advanced imaging techniques are being utilized more frequently to identify inflammation in the colon. Patients are encouraged to maintain a symptom diary, noting the frequency and severity of their symptoms, which can aid doctors in making a timely diagnosis.
Increased awareness and education about UC are crucial. Public health campaigns and social media platforms are playing a pivotal role in disseminating information, helping individuals recognize symptoms sooner and seek medical advice promptly. The emphasis is on not ignoring persistent digestive issues and understanding that early intervention can lead to better management of the condition.
Common Symptoms of Ulcerative Colitis
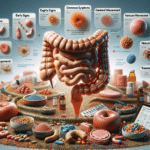
Ulcerative colitis presents a variety of symptoms that can vary in intensity from person to person. The most prevalent symptom is chronic diarrhea, which may be accompanied by blood, indicating inflammation in the colon. Other symptoms include abdominal pain and cramping, often relieved by bowel movements, and a persistent feeling of urgency to use the restroom.
Beyond the digestive system, UC can also manifest in systemic symptoms such as fatigue, fever, and loss of appetite, leading to unintended weight loss. These symptoms can significantly affect an individual’s quality of life, impacting daily activities and overall well-being.
It’s important to note that UC symptoms can fluctuate, with periods of flare-ups and remission. During flare-ups, symptoms become more severe, while remission periods may bring relief. Understanding these patterns can help patients and healthcare providers develop effective management strategies. Keeping track of symptoms and triggers can aid in identifying patterns and tailoring treatment plans to reduce the frequency and severity of flare-ups.
Exploring Treatment Options for Ulcerative Colitis
Treatment options for ulcerative colitis have evolved significantly, offering patients a range of choices to manage their condition. The primary goal of treatment is to reduce inflammation in the colon, alleviate symptoms, and achieve long-term remission. Medications are often the first line of treatment, with options including aminosalicylates, corticosteroids, and immunomodulators.
Biologic therapies have become a cornerstone in UC treatment, particularly for individuals who do not respond to conventional medications. These therapies target specific proteins in the immune system to reduce inflammation. Recent advancements have introduced biosimilars, offering more cost-effective options without compromising efficacy.
In severe cases, surgical interventions may be necessary. Procedures such as colectomy, where part or all of the colon is removed, can provide relief for patients who do not respond to other treatments. However, surgery is typically considered a last resort after exploring other options.
Alongside medical treatments, lifestyle modifications play a crucial role in managing UC. Dietary changes, stress management techniques, and regular exercise can complement medical treatments and help maintain remission. Patients are encouraged to work closely with their healthcare providers to develop a comprehensive treatment plan tailored to their specific needs and lifestyle.